
Not long after the corona pandemic swept across the globe, TU/e began the Covid Engineering Fund. The contributions of donors benefit several ground-breaking research projects.
In one of these promising studies, scientists detect viruses and antibodies using light. This research is able to take place at TU/e because the university is home to many different disciplines on one campus, such as physics, chemistry and biology.
We spoke to some of the people behind these projects:
Prof.dr. Andrea Fiore works within the Department of Applied Physics at TU/e. He is also Scientific Director of the TU/e Institute for Photonic Integration. His main areas of expertise are nanophotonics and quantum photonics.
Prof.dr. Maarten Merkx works within the Department of Biomedical Engineering. He is the Dean of the department and leads the Protein Engineering research group, which operates at the intersection of chemical and synthetic biology.
Dr. Zijlstra works within the Department of Applied Physics. He focuses on Molecular Plasmonics. He develops methods to detect and study individual molecules using light microscopy.
You represent multiple disciplines within science. How unusual is it that you’re working together in this field?
Maarten: “Andrea and Peter are specialists in photonics, which brings together elements from physics and technology, and I’m involved in biochemistry. Indeed, it’s not a standard collaboration. At many universities, you don’t find these disciplines collaborating with each other. However at TU/e, we’ve been working together for a long time. This is mainly thanks to our institutes, which we set up here a number of years ago: ICMS, the Institute for Complex Molecular Studies, and IPI, the Institute for Photonic Integration. Thanks to these institutes we found each other! We exchange knowledge and teach ‘each other’s’ students. This brings new insights and fresh perspectives.”
“We want to detect antibodies and viruses with the help of light.”
What are you working on now?
Andrea: “On fast and inexpensive methods for detecting viruses and antibodies using light, which we do in two ways. The first is using luminescent proteins and the second is developing new photonic chips.”
How does the first method work?
Maarten: “We develop luminescent sensor proteins that change color when they bind to a virus or an antibody. These sensor proteins contain an enzyme that fireflies also use to produce light, but in our case this enzyme comes from a deep-water shrimp. The color of the light then changes from green to blue, which we can measure with a standard digital camera on a cell phone, for instance. With this method, the magic lies in (bio)chemistry.”
And the second method?
Andrea: “Here, we place a layer with ‘capture molecules’ on a sensor surface. These molecules capture, for example, the antibodies we want to detect from a drop of liquid and retain them. We measure this process from a distance by exposing the surface. Such photonic sensors can accurately measure changes in light, even if that light is not visible to the human eye. They measure minuscule changes in the color and intensity of the light reflected from the sensor. From the values we get back, we can see if there are antibodies in the liquid.”
How do your methods compare to existing corona tests?
Maarten: “Firstly, we have to explain how these tests work. There are three types:
The gold standard Corona test is the PCR test, which uses RNA – the DNA of the virus. The RNA sequence was quickly worked out in China.. PCR tests like these are sensitive and specific to certain diseases. However, the required infrastructure and expertise to process them are expensive. Testing can only be done through laboratories therefore the timelines for getting results can be quite long.
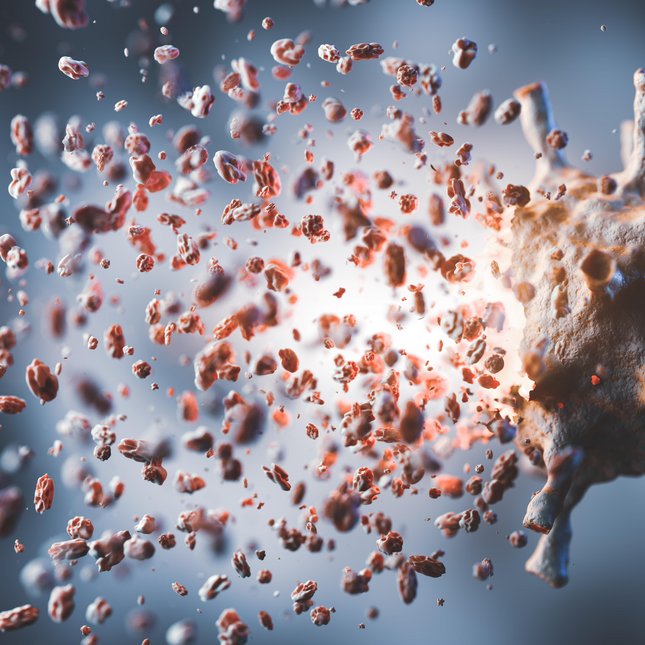
The second test method is the antigen test. This also looks at the virus and specifically at the proteins that the virus carries – like the spike protein, the bulges on the outside of the virus that everyone knows from the images of the coronavirus. These are the quick tests that are performed in the same way as home pregnancy tests. The antigen tests are less sensitive than the PCR tests and can only be used at the peak of the infection.
The third method looks at the immune response. You check blood or saliva for the presence and/or the number of antibodies working against the coronavirus.
Our methods can make the second and third methods faster and more sensitive. If it works, we will very quickly see how many virus particles and antibodies a sample has and which kind they are. This gives us the optimal combination of speed and accuracy. This is ideal in situations, like pandemics, when you want to keep everything under control and therefore want to test quickly.”
These methods use a rod or other simple means to take a sample. How does that work in your projects?
Maarten: “We’re working towards a kind of test strip or a small device on which you can place saliva or a drop of blood, for example. Above all, we want to make it accessible. The beauty of such strips is that we can make several of them with which you can test for different antibodies. And all with the same device or maybe even your cell phone.”
Were you doing this research before corona emerged?
Peter: “Yes we were, although corona has speeded things up. This is also true, of course, in regard to a focus on detecting the specific antibodies involved. For each antibody, you need a different target or receptor molecule. But the techniques lend themselves to the detection of many types of biological molecules, such as antibodies.”
Do you want to develop your own technique for measuring light?
Andrea: “Existing devices with which we measure light, the so-called spectrometers, are very expensive. This is inevitable as they are made to measure many types of light. But for our method, we only need a very limited spectrum. That’s why we want to see if we can develop less complicated and therefore cheaper techniques.”
Why is the price of this technique so important?
Maarten: “You want to be able to test quickly and on a large scale, especially when a pandemic breaks out. If your equipment is too expensive, that won’t happen. That’s why we want to make it accessible to a lot of people. Ideally, we would like to see our technology with every general practitioner in the near future: one device with a selection of relevant test strips for different types of viruses and antibodies. Perhaps even at the homes of consumers or patients too. Not only for corona or the next pandemic but also for the rapid detection (or ruling out) of other diseases.”
That brings us to the following question: you were already working on this and you are now focusing on the pandemic. But what will your world look like after corona?
Peter: “If we develop these techniques further, we will be able to test much faster, easier and in a more focused manner in a few years’ time. Of course, the use is not limited to corona but can also be of added value for other medical conditions.”
“Our tests must be accessible to a lot of people.”
Maarten: “For example, everyone currently gets the same amount of medication for a certain disease profile. However whilst one person may require a high dose of a medication to combat the disease, another person may be able to fight the illness with a much lower dose. Using our testing methods we can personalize and tailor dosage to each patient, thus saving costs and sparing patients from having to take higher than necessary doses of drugs.”
Finally, where do you find the right proteins for the tests?
Peter: “We ‘simply’ take a large part from nature and adapt them where necessary. You can find them in fireflies, for example. Fun fact: for one of the tests, we use proteins from shrimp that live at a depth of five kilometers. If they feel threatened, they emit a very bright blue flash. We like that idea: that we can use a biological phenomenon from a world unknown to us for such a beautiful purpose.”